
Engaging surgeons to assist in contracting for their implants has long been a challenge for most hospitals. Historical feedback from surgeons ranges from “it’s not my problem” to “I’ll just take may cases across the street if I cannot use my vendor of choice.” Presently, organizations may now offer surgeons co-management, value-based, and gainsharing arrangements, as well as other forms of contractual alignments with hospitals. These new business models have proven useful in bringing better balance to the surgeon-hospital relationships vs the traditional surgeon-vendor relationship.
So, how do you engage your surgeons?
Prior to meeting with the surgeons and before sending contracts to the vendor, collecting data to educate your surgeons on current pricing is a critical first step. Creating a surgeon implant profile provides a visualization of vendor selection, type of implant, and total case costs. Typically, this data is not available from a single source but is a custom-crafted database created from multiple hospital data sources.
Below is an example of a surgeon profile for anterior cervical fusions:
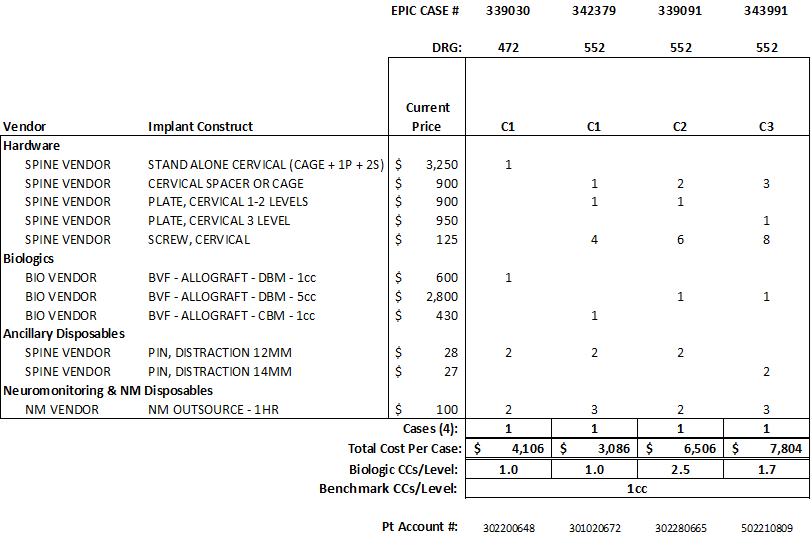
A surgeon implant profile should be as detailed as possible to accurately reflect the surgeon’s practice and product selection. In this example, data is pulled from three different data sources: Operating Room Information System (ORIS), Materials Management Information System (MMIS), and discharge data from finance. Having common data elements across your data, such as the patient account number, is critical.
You never get a second chance at a first impression. Reviewing the combined data for accuracy is the most important part of this process. If the data is not accurate, you will lose credibility instantly with the surgeons. Data should be audited for missing implants, waste, and incorrect pricing. Does the case look correct? Where do you look for data points? Post op notes can provide the implants used and confirm the procedure performed. The implant log in the ORIS can confirm quantity implanted and waste. Verifying the purchase order in MMIS can also confirm implants used, quantity, and price.
Meeting the surgeon is a Who/What/When/Where scenario.
“Who” typically consists of two people:
- The Project Lead – the person who has the best understanding of the data, implants, and procedures performed; and,
- The person who has the best relationship with the surgeons, which may not be the same person for each surgeon. For the initial meeting(s), you may require someone present from the C-Suite or a credible leader the surgeon trusts.
“What” are the goals for the initial meeting?
Communicate your purpose – “We are set to renew our implant contracts and want to ensure we understand your implant selection and preferences.” Start with reviewing their profile and explaining the graphs. Sample questions to ask the surgeon include:
- Does this accurately portray your product selection?
- Do you plan to utilize any different technologies and/or procedures in the future?
- Would you consider utilizing a less expensive comparable product from your vendor?
- Would you switch to another vendor should your current vendor not participate in lowering costs?
You could also share the hospital’s target pricing along with your benchmark pricing so the surgeon can see how their technology currently compares.
“When” and “Where” and how often do you meet with the surgeon? The initial meeting should take no longer than 15-30 minutes and should be scheduled at the surgeons’ convenience – whether their office, before/after their cases, or another location.
Communication is key to a successful surgeon engagement. Consistently following up with surgeons goes a long way in establishing positive ongoing relationships. Providing surgeon implant profiles on a monthly/quarterly basis keeps the surgeons engaged and willing to participate in current CVAT projects and assist future contracting efforts.
For more information, please contact Kim Nilsson at KNilsson@AskPHC.com or 980-721-2637, or John Ossowski at JOssowski@AskPHC.com or 801-209-3304 or Andrew Arreola at AArreola@AskPHC.com or 480-510-7940.

