
(Based on the July 7, 2022 Proposed Rule)
Rate and Conversion Factors
With the budget neutrality adjustments and the required statutory update to the conversion factor for CY 2023 of 0% and the expiration of the 3% increase in PFS payments for CY 2022, the proposed CY 2023 PFS conversion factor is $33.08, a decrease of $1.53 (4.4%) to the CY 2022 PFS conversion factor of $34.61.
Updated Medicare Economic Index (MEI) for CY 2023
CMS is proposing to rebase and revise the MEI cost share weights for CY 2023 as well as a new methodology for estimating base year expenses that relies on publicly available data from the U.S. Census Bureau NAICS 6211 Offices of Physicians.
Evaluation and Management (E/M) Visits
After implementation of the 2021 Outpatient E/M guidelines, the CPT Editorial panel revised the remaining E/M codes. CMS has proposed to adopt these changes in 2023. The changes represent a complete overhaul of the remaining E/M codes to align them with the methodology of the outpatient E/M codes. Key changes include:
- Elimination of the use of history and examination to determine the code level. Instead, there would be a requirement for a medically appropriate history and exam.
- Revising the medical decision-making table from the 2021 guidelines to accommodate all types of E/M services.
- Allowing providers to choose between medical decision making or time to select code level (except for a few code categories such as emergency department visits).
- Consolidating inpatient and observation care into a single code set.
- Consolidating home and domicile care into a single home or residence-based services code set, which would cover assisted living facilities, group homes, custodial care facilities and residential substance abuse treatment facilities.
- CMS will not be adopting the AMA’s prolonged service codes but will be creating their own G codes instead. There will be three, one for inpatient/observation, one for nursing facility, and one for home/resident visits.
- CMS will not be adopting the general CPT rule where the billable amount of time is met once the mid-point is passed. Look for time thresholds from CMS to differ from the AMA’s.
Split (or Shared) E/M Visits
For CY 2023, CMS is proposing to delay the requirement that only time may be used to define “substantive portion” of a split (or shared) visit. Providers will still be able to use history, exam, medical decision making or time to define the “substantiative portion” of a split (or shared) visit.
Telehealth Services
For CY 2023, CMS is proposing to continue several telemedicine flexibilities that were temporarily allowed during the public health emergency (PHE). They are proposing that these “flexibilities” be allowed for 151 days after the end of the PHE to collect data to determine if they will make any of these changes permanent after CY 2023.
- Allowing telehealth services to continue to be provided in any geographic location, including the beneficiary’s home.
- Allowing certain telehealth services to continue to be performed via audio-only device.
- Allowing physical therapists, occupational therapist, speech language therapists, and audiologists to provide telehealth services.
- Delaying the in-person visit requirements for mental health services furnished via telehealth.
- Allowing providers to continue to report telehealth services using the place of service (POS) where the service would normally occur instead of POS 02.
- Allowing providers to continue to report telehealth services with modifier 95.
- Delaying the requirement to report modifier 93 for audio only telehealth services.
Behavioral Health Services
CMS is proposing to create a new code for 2023 that will allow clinical psychologists (CP) or clinical social workers (CSWs) to personally perform and bill general behavioral health integration (GBHI) services. They are also proposing to allow a psychiatric diagnostic evaluation to serve as the initiating visit for the new general BHI service.
In addition, CMS is proposing to make an exception to the direct supervision requirement under the “incident to” regulation to allow behavioral health services provided under the general supervision of a physician or NPP, rather than under direct supervision.
Chronic Pain Management Services
CMS proposes to define chronic pain as persistent or recurrent pain lasting longer than three months and are proposing 2 new HCPCS codes (GYYY1 and GYYY2), for chronic pain management and treatment services (CPM) for CY 2023.
Opioid Use Disorder (OUD) and Opioid Treatment Programs (OTPs)
For CY 2023 and subsequent years, CMS proposes to revise its methodology for pricing the drug component of the methadone weekly bundle (HCPCS codes G2067 and G2078). The proposed CY 2023 methadone payment amount would be $39.29, which is a 5.1 percent increase from 2022 rates. Additionally, for the nondrug component, CMS proposes to update the base rate for individual therapy from 30 to 45 minutes, raising the 2020 base rate from $68.47 to $91.18. CMS would then apply the MEI updates for 2021, 2022 and 2023 to this adjusted rate to determine the CY 2023 payment amounts.
Colorectal Cancer Screening
CMS proposes to expand Medicare coverage of colorectal cancer screening in two ways. First, they propose to reduce the minimum payment age to 45 years. They also propose to expand their regulatory definition of colorectal screening services to include screening colonoscopies that are performed to follow up on positive Medicare covered stool-based colorectal screening tests.
Audiology Services
CMS proposes to allow Medicare beneficiaries to have direct access to an Audiologist without a physician referral. They propose to create a new code (GAUDX) that will allow audiologists to provide direct access care for non-acute hearing or assessments unrelated to disequilibrium, or examinations for the purpose of prescribing, fitting or changing hearing aids. This code would only be billed once per every 12 months.
FY 2023 IPPS Payments (Proposed)
CMS proposed to increase operating payment rates by 3.2% for general acute care hospitals paid under the IPPS that successfully participate in the hospital Inpatient Quality Reporting (IQR) program and are meaningful electronic health record (EHR) users.
This reflects the projected hospital market basket update of 3.1%, reduced by a 0.4 percentage point productivity adjustment, and increased by a 0.5 percentage point for a statutorily required documentation and coding adjustment.
The proposed increase in operating and capital IPPS payment rates, partially offset by decreases in outlier payments for extraordinarily high-cost cases, will generally increase hospitals’ payments in FY 2023 by $1.6 billion.
FY 2023 Physician Fee Schedule (Proposed)
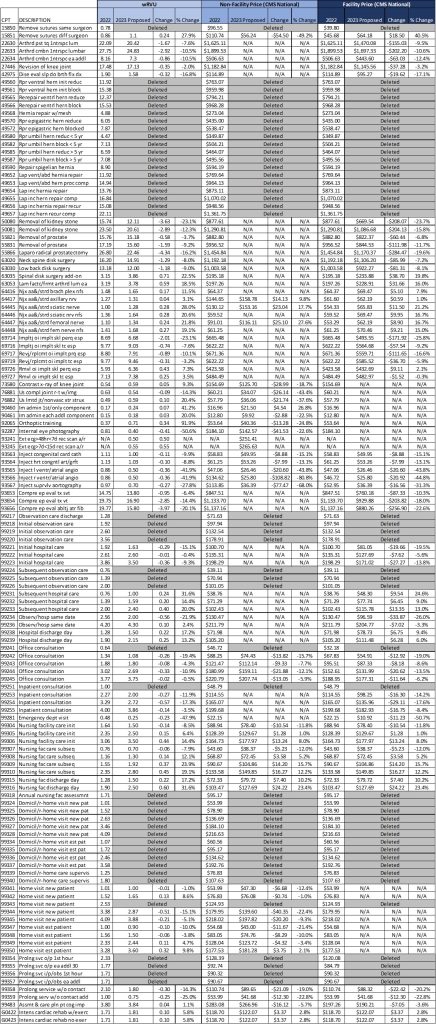
The wRVU and reimbursement rates changed for select procedures in the 2023 proposed rule. Some specialties will be impacted more significantly than others, with a notable reduction in the reimbursement for several cardiovascular services.
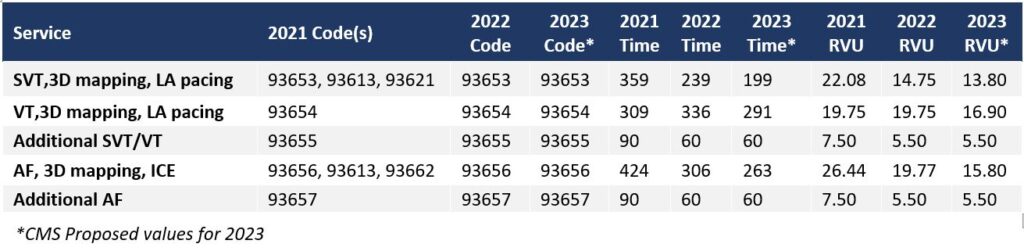
Comparing Cardiac Ablation Coding FY2021 – Proposed FY2023
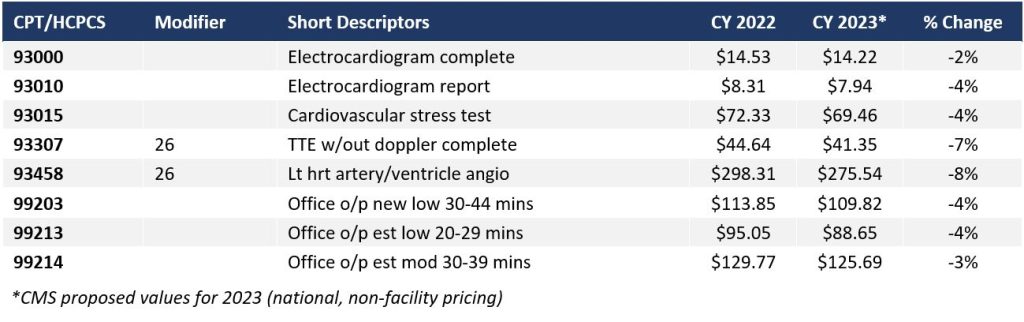
Impact on CY 2023 Payments on Cardiovascular Services
Impact on CY 2023 Payment for Selected Procedures
To learn more about these changes or find out more about our organization, please contact:
| Anthony Long, Partner | Jason Baldwin, Sr. Consultant | Lori Carlin, Director | Robin Peterson, Manager |
| 720-370-9800 | 303-520-2654 | 206-399-7792 | 303-902-8186 |
| ALong@AskPHC.com | JBaldwin@AskPHC.com | LCarlin@AskPHC.com | RPeterson@AskPHC.com |


