Introduction
On April 10, 2024, The Centers for Medicare and Medicaid Services (CMS) released the proposed Inpatient Prospective Payment System (IPPS) for Fiscal Year (FY) 2025. Within the release was the proposed mandatory Transforming Episode Accountability Model (TEAM)[1]. In this article we will break down the proposed rule set forth by the Center for Medicare and Medicaid Innovation (CMMI), which is a program that allows policymakers to establish and test new payment delivery and reimbursement models for both Medicare and Medicaid.
The new TEAM model would be based on five (5) 30-day surgical episodes. The mandatory hospital (participant) will continue to bill Medicare Fee-for-Service (FFS) as in prior years; however, will now receive “target pricing” for included episodes of care prior to each performance year. The model will then assess comparisons in the hospitals’ actual FFS spending through target pricing and assessment of performance in three (3) quality measures: hospital readmissions, patient safety, and patient-reported outcomes.
This is another addition to the already established mandatory payment models, including Bundled Payments for Care Improvement (BPCI), Bundled Payments for Care Improvement Advanced (BPCI-A), and Comprehensive Care for Joint Replacement (CJR) models released in July 2023. It is important to note that all comments on the TEAM model are due, along with all the additional IPPS comments, on June 10, 2024.
Based on geographic regions, if the hospital is paid under the IPPS, and hospitals can obtain buy-in from other providers to agreed shared savings payments, the participants would be selected. You may ask yourself, what does this mean for me? This model is following the same cadence as the CMMI released last year, stating they wanted all traditional Medicare patients under some type of ACO [Accountable Care Organization] by 2030. The release of this model is aligning with that goal and will follow some of the same initiatives released in prior years.
When would the model start?
CMMI proposes the model will begin January 1, 2026, and last five (5) years, ending December 31, 2030. This also means that the model will not begin until after the 2024 election. Therefore, the entire model approval will depend on new leadership at CMMI starting January 1, 2025. Remember, we are still under similar bundled payment models, for example, the CJR model which does not expire until December 31, 2024).
Inclusion Criteria
CMS proposes all services included in the IPPS would be included in the episodes. At the time of admission, beneficiaries must meet all below criteria:
- Enrolled in Medicare Part A and B
- Not eligible for Medicare on the basis of end-stage renal disease
- Not enrolled in ANY managed care plan (i.e., Medicare Advantage)
- Not enrolled in any United Mine Workers of American health plans
- Medicare must be the primary payer
The ACO Conundrum
CMMI also proposed that even if beneficiaries are aligned with another model, the episodes are still mandated to be captured under the TEAM model, meaning if hospitals are currently participating in an ACO (or other care model), they would still be required to participate. There have been many questions raised on timing with the main concern being if it’s too soon to start initiating a mandatory model when we are still in the reporting periods for the CJR and BPCI-A models. There are additional considerations solely for the ACO-based participants (hospitals) under the proposed model.
- Waivers – There will be specific waivers under Section 1115A of the Social Security Act. These waivers are similar to the already existing waivers under episode-based payment models. CMMI proposes waiving geographic and originating site Medicare telemedicine requirements (which are currently waived through December 31, 2024) along with the requirement of beneficiaries to have a prior inpatient encounter of no fewer than three (3) consecutive days to be eligible for coverage of inpatient Skilled Nursing Facility (SNF) care.
- Merit-based Incentive Payment System (MIPS) – The model will provide two (2) Alternative Payment Models (APMs):
- Advanced APM where individuals attest to meeting the Certified Electronic Health Record Technology (“CEHRT”) criteria for qualifying participants (QP) determinations.
- A non-Advanced APM for participants who do not meet the CEHRT criteria.
- Capturing Health Equity Measures – CMMI has also proposed participants would be required to screen beneficiaries for Social Determinants of Health (SDoH) in the following categories:
- Food insecurity
- Housing instability
- Transportation needs
- Utilities difficulties
- Core-Based Statistical Area (CBSA) with average spend included under the BPCI-A data from 1/1/2022-6/30/2023. Provider clinical documentation and the buy-in of the additional participating providers in the ACOs must stratify reportable diagnosis codes.
- Some diagnoses included in the CBSA:
- Chronic Obstructive Pulmonary Disease
- Bronchitis
- Asthma
- Renal Failure
- Sepsis
- Risk Adjustment Normalization
- Coefficients under the risk adjustment model will be calculated at the MS-DRG / CPT® episode level type.
- The same age brackets for risk adjustment (<65, 65-75, 75-<85, 85>) based on the participant’s age at the first date of the episode as determined through Medicare enrollment data will be used.
- A Hierarchical Condition Category (HCC) count risk adjustment variation. This will be considered the TEAM HCC count and will require a 90-day review for each beneficiary, starting with the day prior to the hospitalization or procedure. Following the same FFS under the BPCI-A model, HCC flags all of the FFS claims to determine how to count the HCC diagnosis codes.
- CMS is proposing to expand risk adjustment markers that account for social risk. Even though CMS allows a 1=Y and 2=N rule, the variable would still represent the addition of the three potential markers of beneficiary social risk.
- CMS is considering assigning a value of Y=1 for social risk adjustment variables if the beneficiary falls into a state (8th percentile) or national Area Deprivation Index (ADI), 80th percentile, and / or they qualify for Medicare Part D Low Income Subsidy (LIS).
- CMS is proposing the provision of prospective normalization factors with target prices. The prospective normalization factor is subject to limited adjustment reconciliation and is based on the case mix, up to +/- 5%.
- Some diagnoses included in the CBSA:
Health Equity and Reporting Requirements
CMMI and CMS both proposed under the TEAM model participants can report Health Equity and Reporting Requirements, which will be voluntary in the 1st performance year. In the 2nd performance year, the capture will be mandatory and they must submit a Health Equity Plan. All health equity plans must include the following:
- Health Disparities, including preventable disease burden, injury, violence, and / or opportunities established to assist in achieving optimized health and health outcomes experienced by one or more underserved communities. This element also includes the requirement of how participants aim to reduce health disparities that are identified.
- Health Disparities must also be noted in the plan of care, which includes:
- Health equity goals and how the participant will use goals to monitor and evaluate progress
- Description of health equity plan intervention strategies
- Identification of performance measures, data sources, and equity performance
- Establishment of measures under one or more quantitative metrics that will be used to change health disparities identified in the health equity plan interventions
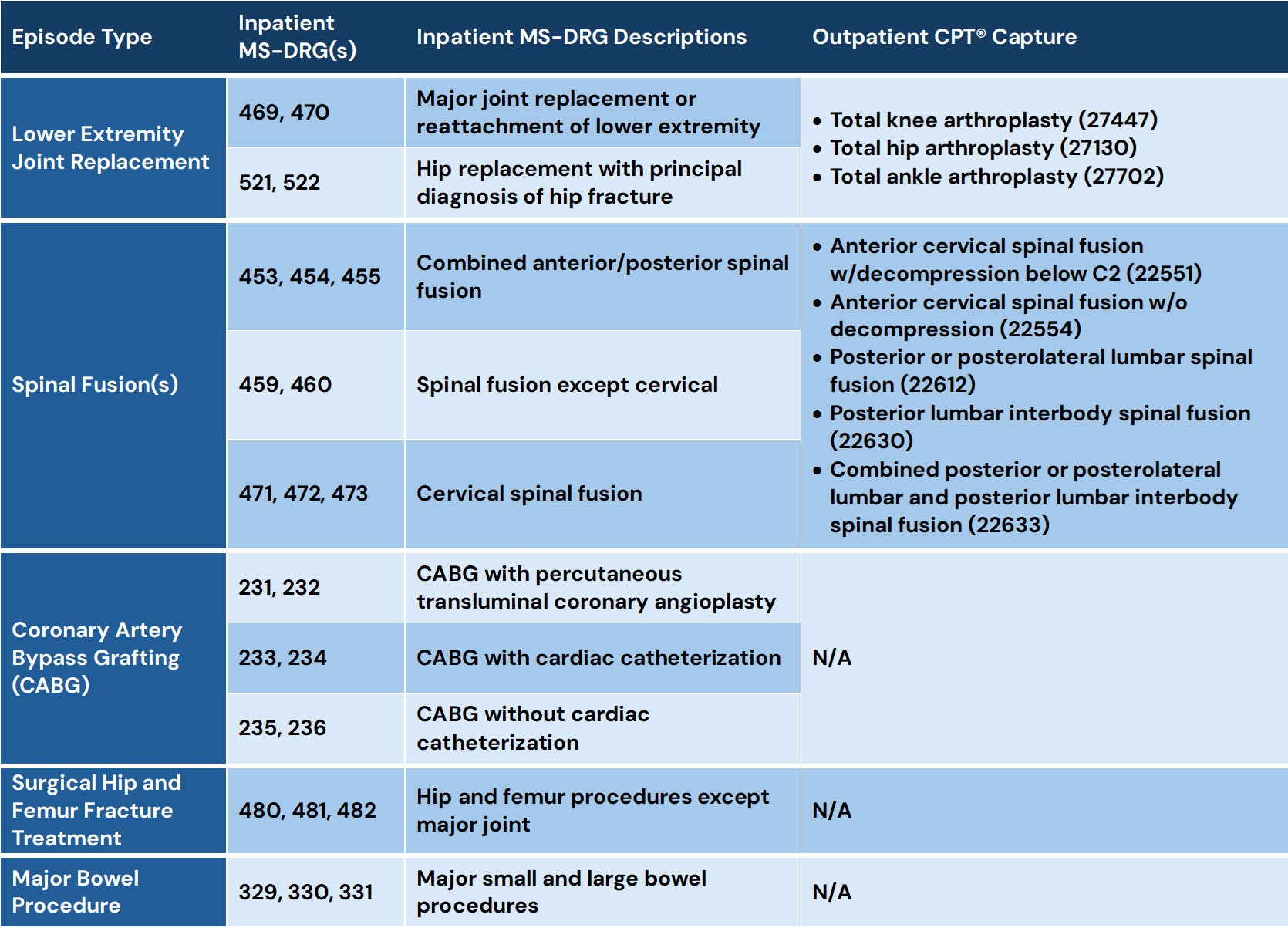
What Procedures Are Included in the TEAM Model and How “Episodes” Are Defined
- Coronary Artery Bypass Grafting (CABG)
- Lower Extremity Joint Replacement (LEJR)
- Surgical Hip and Femur Fracture Treatment (SHFFT)
- Spinal Fusion(s)
- Major Bowel Procedure(s)
Excluded Items Under the “Anchor” Procedure Defined as Unrelated
- Hospital readmissions for specified conditions:
- Oncology
- Trauma
- Organ transplant
- Ventricular shunts
- Major Diagnostic Categories (MDCs):
- 02= Diseases and Disorders of the Eye
- 14= Pregnancy, Childbirth, and Puerperium
- 15= Newborns
- 25= Human Immunodeficiency Virus (HIV)
- New Technology add-on payments for drugs, Outpatient Prospective Payment System (OPPS) pass-through payments for devices classified with status indicator H
- Included on a bill with J1 service
- Pass-through Device Categories (Separate cost-based pass-through payment); Not subject to coinsurance
- Paid at 85% of hospital’s usual and customary charge for the device when properly billed with another Healthcare Common Procedural Service (HCPCS) code if required under the OPPS.
- Certain Part B payments for drugs and biologicals classified as:
- Low Volume (billed for fewer than 31 episodes)
- High-Cost (mean greater than $25,000.00 per episode of care)
- Patients with hemophilia or blood clotting factors paid outside established MS-DRGs, billed on an outpatient claim, and are classified as Durable Medical Equipment (DME)
Financial Risk and Tracking Years
CMMI has proposed the TEAM “participant” and / or hospital will be financially responsible for the entire episode; moving more into the ACO realm of participation, or establishing a VBC payment model. Under the proposed rule, there are three (3) participation tracks established for “RISK”:
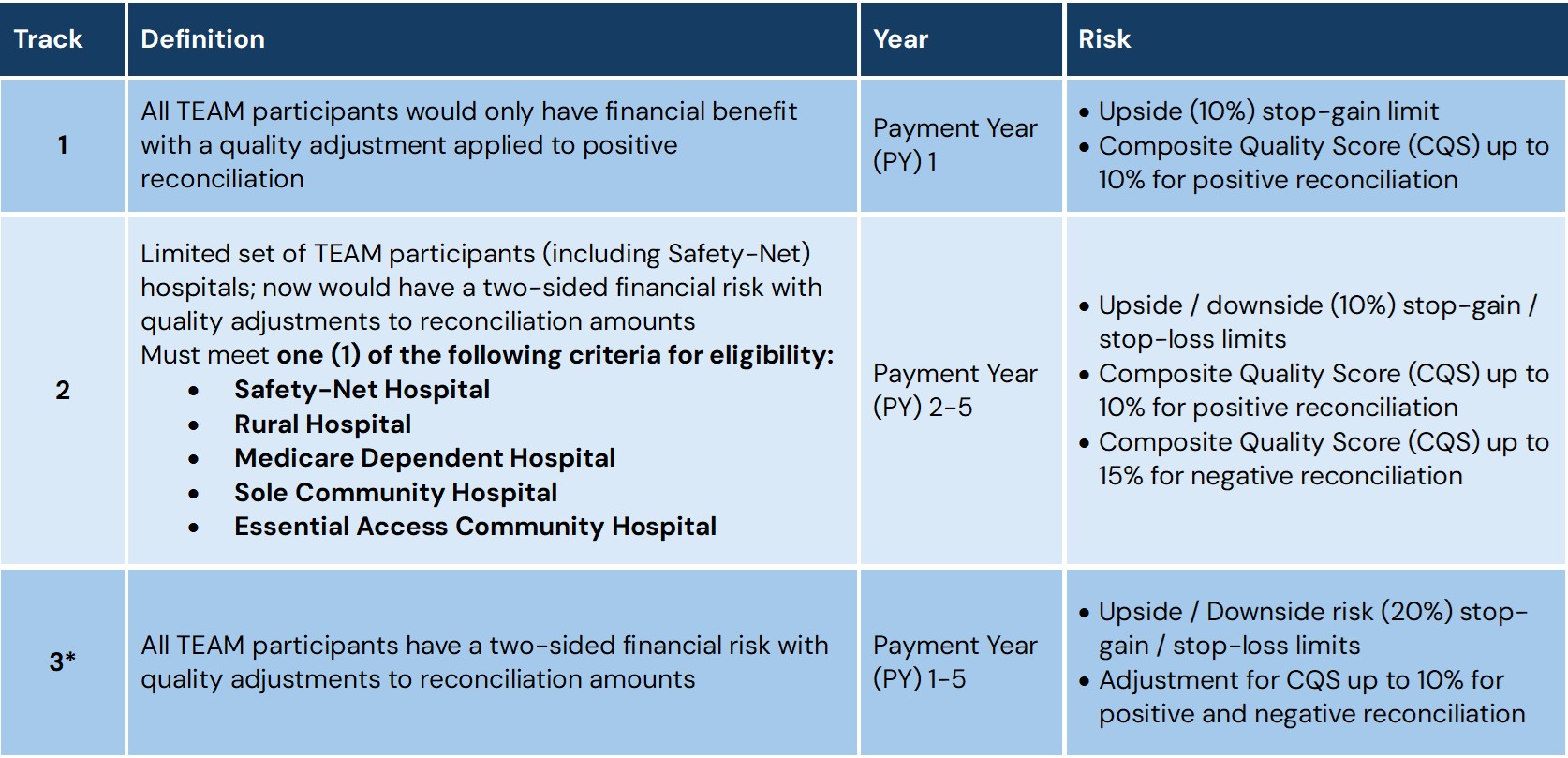
*Track 3 has the highest potential for both savings and losses. There is a maximum up and downside of twenty percent (20%) of the target pricing (“Stop Gain / Stop Loss”).
Quality is KEY!
There are three (3) quality measures being proposed for the TEAM model. CMMI proposes TEAM participant quality should be linked to payment by taking the CQS and adjusting for positive or negative reconciliation amounts. CMMI also notes all quality reporting measures can be documented through existing Hospital Inpatient Quality Reporting (IQR) and / or Hospital Acquired Condition (HAC) programs. There is no additional burden of submitting data. The three (3) IQR measures for ALL TEAM episodes are:
- Hospital-Wide-All-Cause Readmission with Claims and Electronic Health Record Data CMS Measure Inventory Tool (CMIT ID #356)
- CMS Patient Safety and Adverse Events Composite (CMS PSI 90) (CMIT ID# 135)
- Lower Extremity Joint Replacements (LEJR) episodes
- Hospital-Level Total Hip and / or Total Knee Arthroplasty (THA / TKA) Patient-Reported Outcome-Based Performance Measure (PRO-PM) (CMIT ID# 1618)
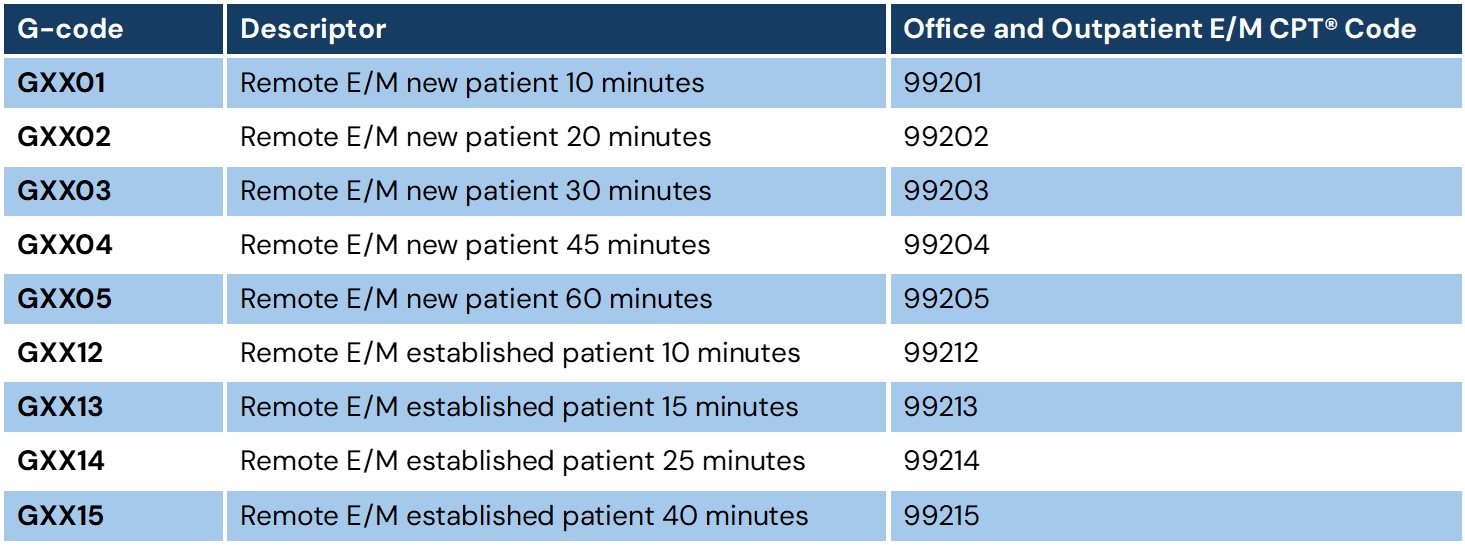
Additionally, CMS has proposed to establish nine (9) new HCPCS G-Codes which will describe Evaluation and Management (E/M) services provided to TEAM beneficiaries in their homes via telemedicine. If the proposed model is finalized, CMS would then specify the G-codes created for the TEAM model and add to the first performance year.
Referrals and Interactions with Other Providers Are Mandatory
All participants / hospitals would be required under the TEAM model to refer patients to a primary care service prior to discharge so they may ensure continuity of care, along with positive long-term outcomes. The model is also providing hospitals with an “option” to team up (ACO / VBC) with other providers to share in the financial risk / savings.
Summary
The TEAM model is aimed at improving care quality for beneficiaries with Medicare to reduce rehospitalization and recovery times of patients undergoing certain high-expenditure, high-volume surgical procedures. By initiating the TEAM model, participant hospitals will not be “accountable” for the quality and cost associated with the procedures which drive outcomes. Hospitals which are required to bill under Medicare FFS would continue to do so; however, would receive a “target” price based on non-exclusions from the Medicare Part A and B services as well as items included in the episode. If the hospital participant is below targeting price, they may have a potential to earn through the quality performance adjustment. Meanwhile, if the hospital participant is above target price, they may owe CMS a repayment for spending beyond the established target price.
It is important to remember the definition of an “episode” includes inpatient hospital services, physician services (including specialists and primary care), outpatient therapy, skilled nursing facilities, home health agencies, clinical laboratory, durable medical equipment, medications (Part B drugs and biologicals), and hospice care.
With all of the new models being released with the initiative of having all traditional Medicare patients under some type of ACO by 2030, we are going to continue to see additional models released. If you are having difficulties keeping up with the changes or would like to know how the changes will affect your organization, please contact Amy Pritchett (APritchett@AskPHC.com) or Kristen Taylor (KTaylor@AskPHC.com) for a consultation.
[1] https://www.cms.gov/priorities/innovation/innovation-models/team-model
