Article originally published in TEAM Connect August Newsletter.
Introduction
The Transforming Episode Accountability Model (TEAM)[1] was first proposed by the Centers for Medicare and Medicaid Services on April 10, 2024, and finalized July 31, 2025, which included 188 geographical regions and over 700 hospitals. In this article we will break down the rule set forth by the Center for Medicare and Medicaid Innovation (CMMI); which is a program that allows policymakers to establish and test new payment delivery and reimbursement models for both Medicare and Medicaid.
As previously noted within the initial release for comment, TEAM will now be a mandatory Alternative Payment Model (APM), based on episodes of care within acute care hospitals. Coordination of care will allow the initiation of an episode (procedure) to be followed and assumed responsibility for not only the cost of the procedure but, the quality of care the patient receives. The model tracks patients from the surgical procedure (initial episode) through the first thirty (30) days after the patient leaves the hospital.
This is just another addition to the already established mandatory payment models; including Bundled Payments for Care Improvement (BPCI), Bundled Payments for Care Improvement Advanced (BPCI-A), and Comprehensive Care for Joint Replacement (CJR) models, released in July 2023.
Based on geographic regions, if the hospital is paid under the Inpatient Prospective Payment Service (IPPS), and hospitals can obtain buy-in from other providers to agreed shared savings payments, the participants would be selected. You may ask yourself, “What does this mean for me?” We have your answer. This model is following the same cadence as the CMMI released two years ago stating they wanted all traditional Medicare patients under some type of Accountable Care Organization (ACO) by 2030. The release of this model is aligning with that goal and will follow some of the same initiatives released in prior years.
Inclusion Criteria
Hospitals reimbursed under the Inpatient Prospective Payment System (IPPS) were selected based on Core-Based Statistical Areas (CBSAs) and geographical location for testing of the model. The model will track patients who undergo surgical procedures for:
- Lower extremity joint replacement(s)
- Surgical correction of hip and femur fracture(s)
- Spinal fusions
- Coronary artery bypass grafting(s)
- Major bowel procedures
CMS will now provide participants in the model a set “bundled” reimbursement, which will be represented by a target price that accounts for all spending during an episode of care. One of the most important aspects of this model is the entire procedure, including the hospital inpatient and / or outpatient visit will now be bundled into the overall reimbursement. TEAMS has also gone so far as to include certain items and services following discharge from the hospital. This includes services such as skilled nursing facility (SNF) visits and provider follow-up encounters. We have all heard the saying, “without risk there is no reward”, and CCIIO kept to this promise. If the costs associated are below the target price, standards of quality are met, hospitals “may” receive a performance bonus, also known as a Reconciliation Payment. However, if the cost exceeds the target pricing, hospitals could owe CMS if the hospital is in “risk” and/or limited track tier. It is the idea of the TEAMS model that if everyone has accountability regarding cost of procedures, this will in turn provide incentives to participants to improve patient interactions and decrease the possibility of readmission.
As always, there are rules and regulations that we must follow when implementing TEAMS into our already established programs. Included in the time of admission, a beneficiary must meet all criteria below:
- Enrolled in Medicare Part A and B
- Not eligible for Medicare on the basis of end-stage renal disease
- Not enrolled in ANY managed care plan (i.e., Medicare Advantage)
- Not enrolled in any United Mine Workers of America health plans
- Medicare must be the primary payer
The ACO Conundrum
CMMI also implemented the regulation that even if beneficiaries are aligned with another model, the episodes are still mandated to be captured under the TEAM model. This means if hospitals are currently participating in an ACO (or other care model), they would still be required to participate. There have been many questions raised on timing during the initial comment period. One of the main concerns addressed has been, “Is it too soon to start initiating an additional mandatory model when hospitals and other organizations are still actively participating in reporting models and periods for CJR and BPCI-A models?” As with any new implementation, there are additional considerations solely for the ACO-based participants (hospitals) under the proposed model. Additionally, in connection with implementing tracks of participation, there are also numerous other considerations under this model.
- Waivers: Specific waivers under Section 1115A of the Social Security Act must be followed per established guidelines. Fortunately, for those already participating in CJR and BPCI-A model’s waivers are, indeed, similar to the already existing waivers under episode-based payment models.
- CMMI waved geographic and originating site Medicare telemedicine requirements along with the requirement of beneficiaries needing to have a prior inpatient encounter of no fewer than three (3) consecutive days to be eligible for coverage of inpatient SNF care.
- Merit-based Incentive Payment System (MIPS): The model will provide two (2) Alternative Payment Models (APMs):
- Advanced APM where individuals attest to meeting the Certified Electronic Health Record Technology (CEHRT) criteria for qualifying participants (QP) determinations
- A non-Advanced APM for participants who do not meet the CEHRT criteria.
- Capturing Health Equity Measures: CMMI[2] has also implemented voluntary requirements regarding screening of beneficiaries for Social Determinants of Health (SDoH) in the following categories:
- Food Insecurity
- Housing Instability
- Transportation Needs
- Utilities Difficulties
- Core-Based Statistical Area (CBSA) with average spend included under the BPCI-A data from 1/1/2022 – 6/30/2023. Provider clinical documentation and the buy-in of the additional participating providers in the ACOs must stratify reportable diagnosis codes.
-
- Some diagnoses included in the CBSA
-
- Chronic Obstructive Pulmonary Disease
- Bronchitis
- Asthma
- Renal Failure
- Sepsis
-
- Risk Adjustment Normalization
- Coefficients under the risk adjustment model will be calculated at the MS-DRG / CPT® episode level type.
- The same age brackets for risk adjustment (<65, 65-75, 75-<85, 85>) based on the participant’s age at the first date of the episode as determined through Medicare enrollment data will be used.
- A Hierarchical Condition Category (HCC) count risk adjustment variation. This will be considered the TEAM HCC count. It will require a 90-day review for each beneficiary, starting with the day prior to the hospitalization or procedure. Following the same FFS under the BPCI-A model, HCC flags all of the FFS claims to determine how to count the HCC diagnosis codes.
- CMS expanded risk adjustment markers accounting for social risk. Even though CMS allows a 1=Y and 2=N rule, the variable would still represent the addition of the three potential markers of beneficiary social risk.
- CMS also implemented assigning a value of Y=1 for social risk adjustment variables if the beneficiary falls into a state (8th percentile) or national Area Deprivation Index (ADI), 80th percentile and / or they qualify for Medicare Part D Low Income Subsidy (LIS).
- Under provisions of prospective normalization factors with target prices, normalization factor is subject to limited adjustment reconciliation based on the case mix up to +/- 9%
- Some diagnoses included in the CBSA
-
What Procedures Are Included in the TEAM Model and How Are “Episodes” Defined
- Coronary Artery Bypass Grafting (CABG)
- Lower Extremity Joint Replacement (LEJR)
- Surgical Hip and Femur Fracture Treatment (SHFFT)
- Spinal Fusion(s)
- Major Bowel Procedure(s)
Excluded Items Under the “Anchor” Procedure Defined as Unrelated:
- Hospital readmissions for specified conditions:
- Oncology
- Trauma
- Organ transplant
- Ventricular shunts
- Major Diagnostic Categories (MDCs):
- 02 = Diseases and Disorders of the Eye
- 14 = Pregnancy, Childbirth, and Puerperium
- 15 = Newborns
- 25 = Human Immunodeficiency Virus (HIV)
- New Technology add-on payments for drugs, Outpatient Prospective Payment System (OPPS) pass-through payments for devices classified with status indicator H
- Included on a bill with J1 service
- Pass-through Device Categories (Separate cost-based pass-through payment); Not subject to coinsurance
- Paid at 85% of hospital’s usual and customary charge for the device when properly billed with another Healthcare Common Procedural Service (HCPCS) code if required under the OPPS.
- Certain Part B payments for drugs and biologicals classified as:
- Low Volume (billed for fewer than 31 episodes)
- High-Cost (mean greater than $25,000.00 per episode of care)
- Patients with hemophilia or blood clotting factors paid outside established MS-DRGs, billed on an outpatient claim, and are classified as Durable Medical Equipment (DME)
Financial Risk and Tracking Years
TEAM “participants” and / or hospitals will be financially responsible for the entire episode, moving more into the ACO realm of participation, or establishing a VBC payment model. Under the final rule, there are three (3) participation tracks established for “RISK”:
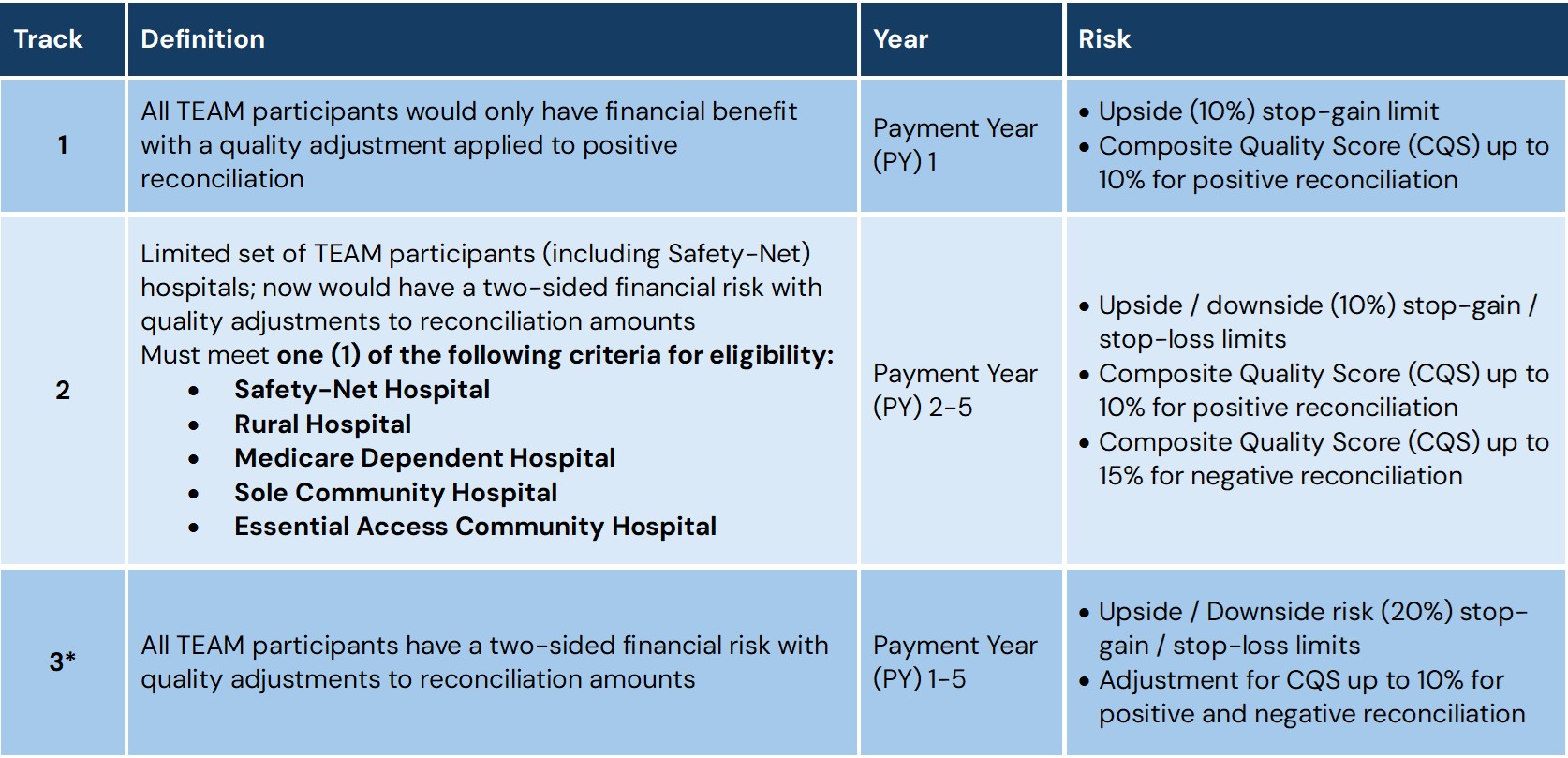
*Track 3 has the highest potential for both savings and losses. There is a maximum up and downside of twenty percent (20%) of the target pricing (“Stop Gain / Stop Loss”).
180-Day Lookback Period for HCC Risk Adjustment
TEAM also implemented a period of “lookback” with the emphasis on collecting information regarding patient’s health history and adjustment to risk factors. This is designed to better capture the beneficiary’s overall health status, while also capturing much needed chronic conditions prior to anchoring to the hospital procedure. Why does the lookback matter:
- The identification of more HCC categories from the patient’s medical history will serve as an accurate process to quantify the expected costs and / or complexities of the patients within the TEAM model to better adjust the cost of care during the episodes.
- Accuracy of the patient’s complete health picture will allow proper setting of the target pricing, in turn better reflecting level of spending, which is outside the control of the hospitals, thus making the lookback period a much needed and equitable pricing methodology by utilizing all of the patient’s medical history.
- The day prior to the anchor procedure being performed is critical as CMS will analyze HCC variables, adjust HCC counts, and flag specific episodes which will be relevant in correct calculation within the regions and directly links to the CBSA capture.
Transition to HCC Version V28: How Will This Impact the TEAM Model?
- Hospitals under the TEAM model will need to account for the lower weights moving from V24 to V28 HCC models. With over 2,500 deletions within the updated V28 model, risk adjustment factors (RAFs) could lead to lower reimbursements for hospitals, especially those in value-based care modeling, including TEAM, CJR, and BPCI-A.
- Implementation of V28 did not come lightly and now demands greater specific in coding to account for the shift in diagnoses and severities. Numerous HCC categories expanded from 3 HCCs to 5 HCCs to further capture conditions that would not otherwise have been captured. We also have to remember that V24 was based on ICD-9-CM methodology and did not account for expansion to ICD-10-CM methodology. Therefore, clear and concise documentation will drive the TEAM model into a very profitable, or very unprofitable risk.
- The growing emphasis on V28 placed more focus on capture of chronic conditions such as diabetes, hypertensive heart disease, and extended into many mental health disorders. Directly fitting into the TEAM model, these diagnoses when captured appropriately will allow providers to further address all chronic conditions and drive better outcomes.
- Although we saw a significant decrease in HCCs from V24 to V28, we also saw the increase of HCC categories from 86 to 115. The utilization of Principle 10 eliminated numerous diagnosis codes that were acute, driven by medications, and even those that were Not Otherwise Specified (NOS), Not Elsewhere Classified (NEC), and Unspecified codes to non-HCCs. The implementation of V28 also came with the deletion of many codes that did not predict future costs of caring for patients within the population.
As we have all seen over the past several months, the Office of Inspector General (OIG) has raised concerns regarding risk adjustment and HCC capture. With the increase in scrutiny over practices, guidelines, and code capture procedures, it is imperative hospitals moving to a TEAM model perform Risk Adjustment Validation (RADV) audits, along with HCC “sweeps” to extrapolate risk. Another important piece of the puzzle within the transition to V28 has been the need for strict adherence to all CMS guidelines and ICD-10-CM Official Guidelines for Coding and Reporting.
Quality is KEY!
There are three (3) quality measures implemented into the TEAM model. TEAM participants quality should be linked to payment by taking the CQS and adjusting for positive or negative reconciliation amounts. CMMI also notes all quality reporting measures can be documented through existing Hospital Inpatient Quality Reporting (IQR) and / or Hospital Acquired Condition (HAC) programs; there is no additional burden of submitting data. The three (3) IQR measures for ALL TEAM episodes are:
- Hospital-Wide-All-Cause Readmission with Claims and Electronic Health Record Data CMS Measure Inventory Tool (CMIT ID #356)
- CMS Patient Safety and Adverse Events Composite (CMS PSI 90) (CMIT ID# 135)
- Lower Extremity Joint Replacements (LEJR) episodes
- Hospital-Level Total Hip and / or Total Knee Arthroplasty (THA / TKA) Patient-Reported Outcome-Based Performance Measure (PRO-PM) (CMIT ID# 1618)
Referrals and Interactions with Other Providers are Mandatory
All participants / hospitals are required under TEAMS to refer patients to a primary care service prior to discharge so they may ensure continuity of care, along with positive long-term outcomes. The model is also providing hospitals with an “option” to team up (ACO / VBC) with other providers to share in the financial risk / savings.
Integration of Quality and Patient Outcomes
Goals under TEAM maintain “simple” costs along with comparisons across geographical regions. TEAM relies on hospital-based performance and quality metrics reporting. CMS will be evaluating hospitals on established clinical criteria and patient-experience measures including:
- Readmission Rates
- Patient-reported outcome measures (PROMs)
- Infection and procedure complication rates
- Health-related patient experience (HCAHPS)
Weighted Volume and Episodes of Care Reporting
Overall quality scores will be calculated utilizing a method CMS calls volume weighting. Simply put, quality scores from all procedures performed frequently will have a larger impact on your overall score. Take for example your hospital carries out 200 joint replacements and 50 coronary artery bypass grafts per year. Within the TEAM model, joint replacements are going to total more of the TEAM episodes than the coronary artery bypass grafts. CMS is now weighing quality scores based on joint replacement metrics at up to three times than coronary artery bypass grafts to determine the final composite scoring. Utilizing this approach to metrics, CMS can validate highest volume procedures carry more influence and reflect the risk impact on quality and cost performance measures.
Summary
The TEAM model is aimed at improving care quality for beneficiaries with Medicare to reduce rehospitalization and recovery times of patients undergoing certain high-expenditure, high-volume surgical procedures. By initiating the TEAM model, participant hospitals will now be “accountable” for the quality and cost associated with the procedures which drive outcomes. Hospitals who are required to bill under Medicare FFS would continue to do so; however, would receive a “target” price based on non-exclusions from the Medicare Part A and B services as well as items included in the episode. If the hospital participant is below targeting price, they may have a potential to earn through the quality performance adjustment. Meanwhile, if the hospital participant is above target price, they may owe CMS a repayment for spending beyond the established target price.
It is important to remember the definition of an “episode” includes inpatient hospital services, physician services (including specialists and primary care), outpatient therapy, skilled nursing facilities, home health agencies, clinical laboratory, durable medical equipment, medications (Part B drugs and biologicals), and hospice care. Hospitals in participating regions should start preparations today for potential implications of the model. The nature of TEAM is mandatory and has been a contentious battle between organizations who are effectively pushing advocation to make the model voluntary. Hospitals will be on a glide path intended to ease hospitals into full financial risk for the first year.
To properly prepare for implementation, hospitals are going to require a multidimensional approach. The main focus should be on analytics, staff coordination and engagement, and leveraging advanced technologies. Baseline performance including analysis of past data performance on the identified surgical episodes will assist in identifying greatest strengths and weaknesses across cost and quality metrics. Remember, the model strongly focuses on readmissions, complications, and patient satisfaction scores. In the upcoming months, it is going to be of the utmost importance to determine volumes and identify financial impact under the new model. Clear goals must be defined early and should focus on measurable goals and its impact to patient outcomes, quality, and cost of services.
Care coordination will be the driving factor of the model. It is crucial to establish communication not only with providers directly involved in patient care but, inclusion of inpatient teams, primary care providers, post-acute care providers, and even home health services and durable medical equipment services. Use of claims data, patient and physician-level costs, and established CMS benchmarks are going to be critical in sourcing and analyzing bundled payment performance. The use of predictive modeling is going to be imperative as the model pushes the envelope between retrospective reporting and simultaneous capabilities to complete performance monitoring along with financial exposure.
Education and engagement is going to be crucial post-implementation. Everyone from clinical to administrative and revenue cycle needs to understand the model, implications, and driven goals towards improvement of patient care, quality outcomes, and cost efficiencies.
With all of the new models being released with the initiative of having all traditional Medicare patients under some type of ACO by 2030, we are going to continue to see additional models released. If you are having difficulties keeping up with the changes or would like to know how the changes will affect your organization, please contact Amy Pritchett (APritchett@AskPHC.com) or Kristen Taylor (KTaylor@AskPHC.com) for a consultation.
[1] https://www.cms.gov/priorities/innovation/innovation-models/team-model
[2] https://www.ecfr.gov/current/title-42/chapter-IV/cubchapter-H/part512/subpart-#/subject-group-ECFRc21831a20f031bd/section-512.563

